Sheryl Shook
Cardiovascular Experiments
Learning Objectives
- Explain the physiological basis for each wave of the electrocardiogram (ECG).
- Demonstrate the procedure for conducting an ECG.
- Identify cardiac cycle components from ECG data.
- Demonstrate the sites and techniques for taking pulse to measure heart rate.
- Compare heart rate values calculated from ECG to those from taking a pulse.
- Demonstrate sphygmomanometry (blood pressure measurement).
Electrocardiogram
By placement of surface electrodes on the body, it is possible to record the complex electrical signal of the heart. This tracing of the electrical signal is the electrocardiogram (ECG), also abbreviated EKG (K for kardiologie in German). Analysis of the ECG reveals a detailed picture of both normal and abnormal heart function. The standard electrocardiograph (the instrument that generates an ECG) uses 3, 5, or 12 leads. The term “lead” may be used to refer to the cable from the electrode on the body to the electrical recorder, but “lead” typically describes the voltage difference between two of the electrodes, as if a “lead” is a view of electrical movement from a specific perspective. A given lead shows how the electrical activity travels through the heart in terms of a particular spatial orientation. For example, a “Lead II” ECG shows how the voltage travels through the heart along the frontal plane. The 12-lead electrocardiograph uses 10 electrodes placed in standard locations on the patient’s skin (see Figure 4.1 below). In this lab we will use only the 4 electrodes, placed on the limbs, with the one on the right leg being the ground. This will allow viewing of Leads I, II, and III (Figure 4.2). The greater the number of leads an electrocardiograph uses, the more information the ECG provides.

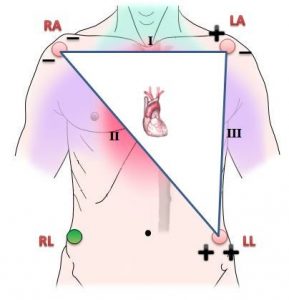
Image derived from “Angina pectoris” by Ian Furst / CC BY-SA 3.0 and “Bipolar electrodes for leads I, II, and III” by Paul Sakuma / CC BY-SA 4.0
We will place our electrodes on the wrists for RA & LA and ankles for RL & LL.
A normal ECG tracing is presented in Figure 4.3. Each tiny square, 1mm, is the passing of 0.04 seconds. Notice there are 25mm every 1 second. You will use this when determining the values on your own ECG today. Segments are defined as the regions between two waves. Intervals include one segment plus one or more waves. Each wave, segment, and interval is related to electrical events associated with various stages of contraction and relaxation of the heart.
- P wave: Depolarization of the atria.
- PR interval: Time for voltage to travel from the SA node, through the atria, and into the ventricles.
- P-R segment: Time for voltage to travel from AV node to ventricles.
- QRS complex: Depolarization of the ventricles. The repolarization of the atria occurs during the QRS complex, which masks it on an ECG.
- S-T segment: Measures the delay between ventricular depolarization and repolarization.
- QT interval: The total time of the ventricular depolarization and repolarization cycle.
- T wave: repolarization of the ventricles.
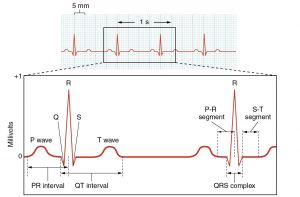
Electrocardiogram by Open Stax / CC BY 4.0. Download for free at Open Stax.
Instructions for ECG
- Gently clean the skin, using alcohol and tissue, on the wrists and medial surface of the ankles in the four limb locations shown in Figure 4.1.
- Apply the electrode pads and clip the appropriate ECG cable to the pad.
- Have your participant sit still with hands relaxed on lap. Place a fabric or paper folder in lap, between thighs and hands, if participant’s hands are touching the skin of the thighs (e.g. wearing shorts).
- Press <9> button to start recording. The machine will print the ECG and stop automatically.
- Label (waves, intervals, etc.) on your ECG and record values for all the items shown in Figure 4.3.
The time between R wave peaks is the time for a cardiac cycle, which is also the time between heart beats. In addition to labeling your ECG, calculate the heart rate (beats per minute) using the number of squares between two consecutive R wave peaks. Write this out on your ECG printout. For example, using Figure 4.3 data, there are 20 tiny boxes (mm squares) between each peak of the R wave and each tiny box represents 0.04 seconds:
20 tiny boxes x 0.04 seconds/1 tiny box = 0.8 seconds between R wave peaks.
Confirm 0.8 seconds looks correct based on the figure. Then:
1 heart beat/0.8 seconds x 60 seconds/minute = 75 beats/minute
Which units canceled out in the above equation?
Heart Sounds, Pulse, and Blood Pressure
Heart Sounds
A stethoscope is often used during auscultation, listening to sounds from body organs such as the lungs or heart. The healthy heart has two sounds, S1 (lub) and S2 (dup).
S1: blood turbulence from closing of atrioventricular valves.
S2: blood turbulence from closing of semilunar valves.
What is directly over the valves (in between the heart and your stethoscope on the chest)? How might this be related to the auscultation sites?
Instructions for Heart Sounds
- Using alcohol and wipes, clean the earpieces and stethoscope diaphragm and allow to dry.
- Rotate the stethoscope earpieces so they will face slightly anterior before placing in your ears.
- Facing your seated and relaxed partner, place the diaphragm of the stethoscope in each of the locations shown in Figure 4.4. Consider allowing your partner to place the stethoscope diaphragm over their own chest if that provides more comfort with the procedure.
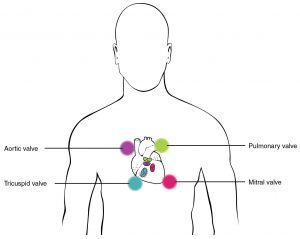
Stethoscope Placement for Auscultation by Open Stax / CC BY 4.0. Download for free at Open Stax.
Pulse
When the left ventricle contracts, creating the systolic pressure, a pressure wave travels through the arteries. This causes expansion and recoil of arteries that can be felt as a pulse at several body points (Figure 4.5).
Instructions for Pulse
- On yourself and a partner, palpate at least three of the pulse sites below to feel confident you can find a pulse.
- Select one site and take your partner’s pulse for 60 seconds. This is the heart rate in beats per minute. When you take the pulse in this manner, is it more or less accurate than using the ECG calculation based on R-R interval? Why?
- Palpate the brachial pulse in preparation for the blood pressure lab that follows.
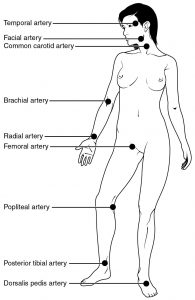
Pulse Sites by Open Stax / CC BY 4.0. Download for free at Open Stax.
Blood Pressure
As the heart contracts and relaxes, it creates a range of pressures against the blood vessel walls. Blood pressure is reported after taking two measurements:
Systolic Blood Pressure (SBP) is the high arterial pressure caused by contraction of the left ventricle. The ideal range is 90-120 mm Hg.
Diastolic Blood Pressure (DBP) is the low arterial pressure resulting from left ventricle relaxation. The ideal range is 60-80 mm Hg
The reading is recorded in this format SBP/DBP, for example 110/70.
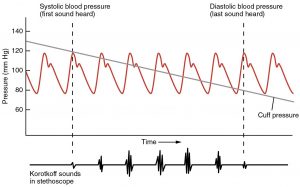
To measure blood pressure, a sphygmomanometer is used. It is a cuff that blocks blood flow, an attached bulb and valve to control pressure, and a pressure dial for reading values (Figure 4.6). When the cuff is wrapped around upper arm and inflated enough to block the blood flow to the lower arm, the pressure is slowly released allowing readings to be taken for SBP and DBP (Figure 4.7). Traditionally this required use of a stethoscope to listen to noise from blood turbulence (Korotkoff sounds) at the brachial artery. Clinically, it is commonly automated and the stethoscope is not necessary.
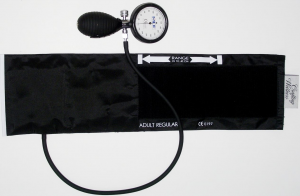
Sphygmomanometer and Cuff / CC0
Blood Pressure Measurement by Open Stax / CC BY 4.0. Download for free at Open Stax.
Instructions for Blood Pressure
Before beginning, view this video on blood pressure deflation rate.
Video 4.1. Blood Pressure – Deflation Rate, Ryerson University / CC BY
- Get comfortable opening and closing the pressure valve so you can hold the bulb and operate the valve easily with one hand. Turning valve to the right closes (right-tight) and turning to the left opens (left-loose). With the valve opened, squeeze all the air out of the cuff.
- With your participant comfortably seated and arm resting on lab table, wrap cuff around the upper arm (brachium), about two fingers above the cubital fossa. The cuff arrow should be positioned over the brachial artery pulse point that you identified in the pulse-taking activity. Verify this positioning by palpating the brachial pulse. Secure the cuff loosely enough that you can just slip two fingers inside between the cuff and the arm. Clip the pressure dial to the loop of the cuff so you can easily read it.
- Place stethoscope earpieces in ears, and with one hand, hold the stethoscope diaphragm in place over the brachial artery (Figure 4.8).
- In the next step you will inflate the cuff. Once the cuff is inflated, do not keep it inflated for more than 1 minute. Also, if you inflate the cuff and have difficulty taking the reading, change arms and start over so the original arm blood flow can reestablish.
- Inflate the cuff to 160 mm Hg, notice you hear no sounds. While watching the pressure dial, slowly release the pressure while listening for the first sound of blood turbulence (Korotkoff sound). Notice and remember the pressure when you first hear the sound. This is the systolic blood pressure (SBP). There is turbulence because the vessel is constricted too much for a quiet smooth flow.
- Continue slowly releasing the pressure as you listen for the instant the sounds go away. Note this mentally as the diastolic blood pressure (DBP). Silence means the blood is flowing smoothly and quietly. Release the rest of the pressure in the cuff and record your values as SBP/DBP.
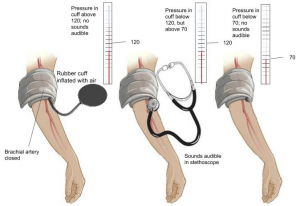
Image by Ashley Kajioka / CC BY 4.0
“Cardiovascular Experiments” is MODIFIED from:
Content on Electrocardiogram is modified from OpenStax College, Anatomy and Physiology.
Download for free at http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@12.8.
