Indicators of Health: Body Mass Index, Body Fat Content, and Fat Distribution
University of Hawai‘i at Mānoa Food Science and Human Nutrition Program and Human Nutrition Program
Although the terms overweight and obese are often used interchangeably and considered as gradations of the same thing, they denote different things. The major physical factors contributing to body weight are water weight, muscle tissue mass, mass, and fat tissue mass. Overweight refers to having more weight than normal for a particular height and may be the result of water weight, muscle weight, or fat mass. Obese refers specifically to having excess body fat. In most cases people who are overweight also have excessive body fat and therefore body weight is an indicator of obesity in much of the population.
The “ideal” healthy body weight for a particular person is dependent on many things, such as frame size, sex, muscle mass, bone density, age, and height. The perception of the “ideal” body weight is additionally dependent on cultural factors and the mainstream societal advertisement of beauty.
To standardize the “ideal” body weight and relate it to health, scientists have devised mathematical formulas to better define a healthy weight. These mathematically derived measurements are used by health professionals to correlate disease risk with populations of people and at the individual level. A clinician will take two measurements, one of weight and one of fat mass, in order to diagnose obesity. Some measurements of weight and body fat that do not require using technical equipment can easily be calculated and help provide an individual with information on weight, fat mass, and distribution, and their relative risk of some chronic diseases.
Figure 2.28 Body Composition

Body Mass Index: How to Measure It and Its Limitations
is calculated using height and weight measurements and is more predictive of body fatness than weight alone. BMI measurements are used to indicate whether an individual may be underweight (with a BMI less than 18.5), overweight (with a BMI over 25), or obese (with a BMI over 30). High BMI measurements can be warning signs of health hazards ahead, such as cardiovascular disease, Type 2 diabetes, and other chronic diseases. BMI-associated health risks vary by race. Asians face greater health risks for the same BMI than Caucasians, and Caucasians face greater health risks for the same BMI than African Americans.
Calculating BMI
To calculate your BMI, multiply your weight in pounds by 703 (conversion factor for converting to metric units) and then divide the product by your height in inches, squared.
BMI = [weight (lb) x 703] ÷ height (in)2
or
BMI = [weight (kg)] ÷ height (m)2
More Ways to Calculate
The National Heart, Lung, and Blood Institute and the CDC have automatic BMI calculators on their websites:
- https://www.nhlbisupport.com/bmi/
- https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/english_bmi_calculator/bmi_calculator.html
To see how your BMI indicates the weight category you are in, see Table 2.3 “BMI Categories”.
Table 2.3 BMI Categories
| Categories | BMI |
| Underweight | < 18.5 |
| Healthy or Normal weight | 18.5–24.9 |
| Overweight | 25–29.9 |
| Obese | > 30.0 |
Source: National Heart, Lung, and Blood Institute. Accessed November 4, 2012. https://www.nhlbi.nih.gov.
BMI Limitations
A BMI is a fairly simple measurement and does not take into account fat mass or fat distribution in the body, both of which are additional predictors of disease risk. Body fat weighs less than muscle mass. Therefore, BMI can sometimes underestimate the amount of body fat in overweight or obese people and overestimate it in more muscular people. For instance, a muscular athlete will have more muscle mass (which is heavier than fat mass) than a sedentary individual of the same height. Based on their BMIs the muscular athlete would be less “ideal” and may be categorized as more overweight or obese than the sedentary individual; however this is an infrequent problem with BMI calculation. Additionally, an older person with (decreased bone mass) will have a lower BMI than an older person of the same height without osteoporosis, even though the person with osteoporosis may have more fat mass. BMI is a useful inexpensive tool to categorize people and is highly correlative with disease risk, but other measurements are needed to diagnose obesity and more accurately assess disease risk.
Body Fat and Its Distribution
Next we’ll discuss how to measure body fat, and why distribution of body fat is also important to consider when determining health.
Measuring Body Fat Content
Water, , bone tissue, fat, and muscle tissue make up a person’s weight. Having more fat mass may be indicative of disease risk, but fat mass also varies with sex, age, and physical activity level. Females have more fat mass, which is needed for reproduction and, in part, is a consequence of different levels of . The optimal fat content of a female is between 20 and 30 percent of her total weight and for a male is between 12 and 20 percent. Fat mass can be measured in a variety of ways. The simplest and lowest-cost way is the skin-fold test. A health professional uses a caliper to measure the thickness of skin on the back, arm, and other parts of the body and compares it to standards to assess body fatness. It is a noninvasive and fairly accurate method of measuring fat mass, but similar to BMI, is compared to standards of mostly young to middle-aged adults.
Figure 2.29 Measuring Skinfold Thickness Using Calipers

Other methods of measuring fat mass are more expensive and more technically challenging. They include:
- Underwater weighing. This technique requires a chamber full of water big enough for the whole body to fit in. First, a person is weighed outside the chamber and then weighed again while immersed in water. Bone and muscle weigh more than water, but fat does not—therefore a person with a higher muscle and bone mass will weigh more when in water than a person with less bone and muscle mass.
- Bioelectric Impedance Analysis (BIA). This device is based on the fact that fat slows down the passage of electricity through the body. When a small amount of electricity is passed through the body, the rate at which it travels is used to determine body composition. These devices are also sold for home use and commonly called body composition scales.
Figure 2.30 BIA Hand Device

- Dual-energy X-ray absorptiometry (DEXA). This can be used to measure bone density. It also can determine fat content via the same method, which directs two low-dose X-ray beams through the body and determines the amount of the energy absorbed from the beams. The amount of energy absorbed is dependent on the body’s content of bone, lean tissue mass, and fat mass. Using standard mathematical formulas, fat content can be accurately estimated.
Figure 2.31 Dual-Energy X-ray Absorptiometry (DEXA)

Measuring Fat Distribution
Total body-fat mass is one predictor of health; another is how the fat is distributed in the body. You may have heard that fat on the hips is better than fat in the belly—this is true. Fat can be found in different areas in the body and it does not all act the same, meaning it differs physiologically based on location. Fat deposited in the abdominal cavity is called visceral fat and it is a better predictor of disease risk than total fat mass. Visceral fat releases hormones and inflammatory factors that contribute to disease risk. The only tool required for measuring visceral fat is a measuring tape. The measurement (of waist circumference) is taken just above the belly button. Men with a waist circumference greater than 40 inches and women with a waist circumference greater than 35 inches are predicted to face greater health risks.
Figure 2.32 Fat Distribution
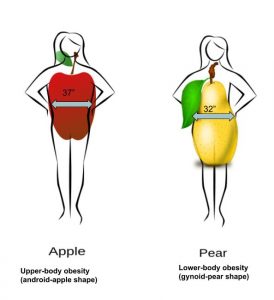
The waist-to-hip ratio is often considered a better measurement than waist circumference alone in predicting disease risk. To calculate your waist-to-hip ratio, use a measuring tape to measure your waist circumference and then measure your hip circumference at its widest part. Next, divide the waist circumference by the hip circumference to arrive at the waist-to-hip ratio. Observational studies have demonstrated that people with “apple-shaped” bodies, (who carry more weight around the waist) have greater risks for chronic disease than those with “pear-shaped” bodies, (who carry more weight around the hips). A study published in the November 2005 issue of Lancet with more than twenty-seven thousand participants from fifty-two countries concluded that the waist-to-hip ratio is highly correlated with heart attack risk worldwide and is a better predictor of heart attacks than BMI.[1]. Abdominal obesity is defined by the World Health Organization (WHO) as having a waist-to-hip ratio above 0.90 for males and above 0.85 for females.
Learning Activities
Technology Note: The second edition of the Human Nutrition Open Educational Resource (OER) textbook features interactive learning activities. These activities are available in the web-based textbook and not available in the downloadable versions (EPUB, Digital PDF, Print_PDF, or Open Document).
Learning activities may be used across various mobile devices, however, for the best user experience it is strongly recommended that users complete these activities using a desktop or laptop computer and in Google Chrome.
- Yusuf S, Hawken S, et al. (2005). Obesity and the Risk of Myocardial Infarction in 27,000 Participants from 52 Countries: A Case-Control Study. Lancet, 366(9497), 1640–9. https://pubmed.ncbi.nlm.nih.gov/16271645/ ↵
The major structural and supportive connective tissue of the body.
A person’s weight in kilograms divided by their height in meters squared.
A disorder affecting the bones that is characterized as a loss in bone mass, increased bone fragility, and increased risk of fractures.
A group of tissues that performs a specialized function.
A chemical messenger in the body that is released into the blood from one specific location in the body and travels to another location, where it elicits a specific response.
