Calcium
Calcium’s Functional Roles
Calcium is the most abundant mineral in the body and greater than 99 percent of it is stored in . Although only 1 percent of the calcium in the human body is found in the blood and soft tissues, it is here that it performs the most critical functions. Blood calcium levels are rigorously controlled so that if blood levels drop the body will rapidly respond by stimulating , thereby releasing stored calcium into the blood. Thus, bone tissue sacrifices its stored calcium to maintain blood calcium levels. This is why bone health is dependent on the intake of dietary calcium and also why blood levels of calcium do not always correspond to dietary intake.
Calcium plays a role in a number of different functions in the body like bone and tooth formation. The most well-known calcium function is to build and strengthen bones and teeth. Recall that when bone tissue first forms during the modeling or remodeling process, it is unhardened, protein-rich osteoid tissue. In the osteoblast-directed process of bone mineralization, calcium phosphates (salts) are deposited on the protein matrix. The calcium salts typically make up about 65 percent of bone tissue. When your diet is calcium deficient, the mineral content of bone decreases causing it to become brittle and weak. Thus, increased calcium intake helps to increase the mineralized content of bone tissue. Greater mineralized bone tissue corresponds to a greater BMD, and to greater bone strength. The remaining calcium plays a role in nerve impulse transmission by facilitating electrical impulse transmission from one nerve cell to another. Calcium in muscle cells is essential for muscle contraction because the flow of calcium ions are needed for the muscle proteins (actin and myosin) to interact. Calcium is also essential in blood clotting by activating clotting factors to fix damaged tissue.
In addition to calcium’s four primary functions calcium has several other minor functions that are also critical for maintaining normal physiology. For example, without calcium, the hormone could not be released from cells in the pancreas and glycogen could not be broken down in muscle cells and used to provide energy for muscle contraction.
Maintaining Calcium Levels
Because calcium performs such vital functions in the body, blood calcium level is closely regulated by the hormones (), calcitriol, and . When blood calcium levels are low, PTH is secreted to increase blood calcium levels via three different mechanisms. First, PTH stimulates the release of calcium stored in the bone. Second, PTH acts on kidney cells to increase calcium reabsorption and decrease its excretion in the urine. Third, PTH stimulates in the kidney that activate to calcitriol. Calcitriol is the active hormone that acts on the intestinal cells and increases dietary calcium absorption. When blood calcium levels become too high, the hormone calcitonin is secreted by certain cells in the and PTH secretion stops. At higher nonphysiological concentrations, calcitonin lowers blood calcium levels by increasing calcium excretion in the urine, preventing further absorption of calcium in the gut and by directly inhibiting bone resorption.
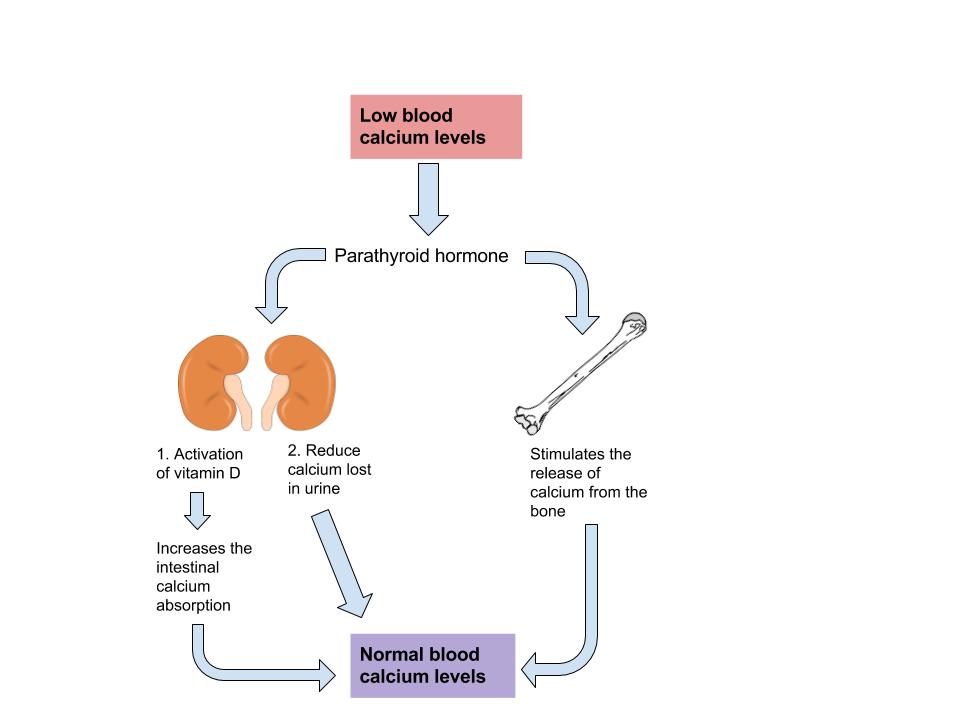
Image by Allison Calabrese / CC BY 4.0
Other Health Benefits of Calcium in the Body
Besides forming and maintaining strong bones and teeth, calcium has been shown to have other health benefits for the body, including:
- Cancer. The National Cancer Institute reports that there is enough scientific evidence to conclude that higher intakes of calcium decrease colon cancer risk and may suppress the growth of polyps that often precipitate cancer. Although higher calcium consumption protects against colon cancer, some studies have looked at the relationship between calcium and prostate cancer and found higher intakes may increase the risk for prostate cancer; however the data is inconsistent and more studies are needed to confirm any negative association.
- Blood pressure. Multiple studies provide clear evidence that higher calcium consumption reduces blood pressure. A review of twenty-three observational studies concluded that for every 100 milligrams of calcium consumed daily, systolic blood pressure is reduced 0.34 millimeters of mercury (mmHg) and diastolic blood pressure is decreased by 0.15 mmHg.[1]
- Cardiovascular health. There is emerging evidence that higher calcium intakes prevent against other risk factors for cardiovascular disease, such as high cholesterol and obesity, but the scientific evidence is weak or inconclusive.
- Kidney stones. Another health benefit of a high-calcium diet is that it blocks kidney stone formation. Calcium inhibits the absorption of oxalate, a chemical in plants such as parsley and spinach, which is associated with an increased risk for developing kidney stones. Calcium’s protective effects on kidney stone formation occur only when you obtain calcium from dietary sources. Calcium supplements may actually increase the risk for kidney stones in susceptible people.
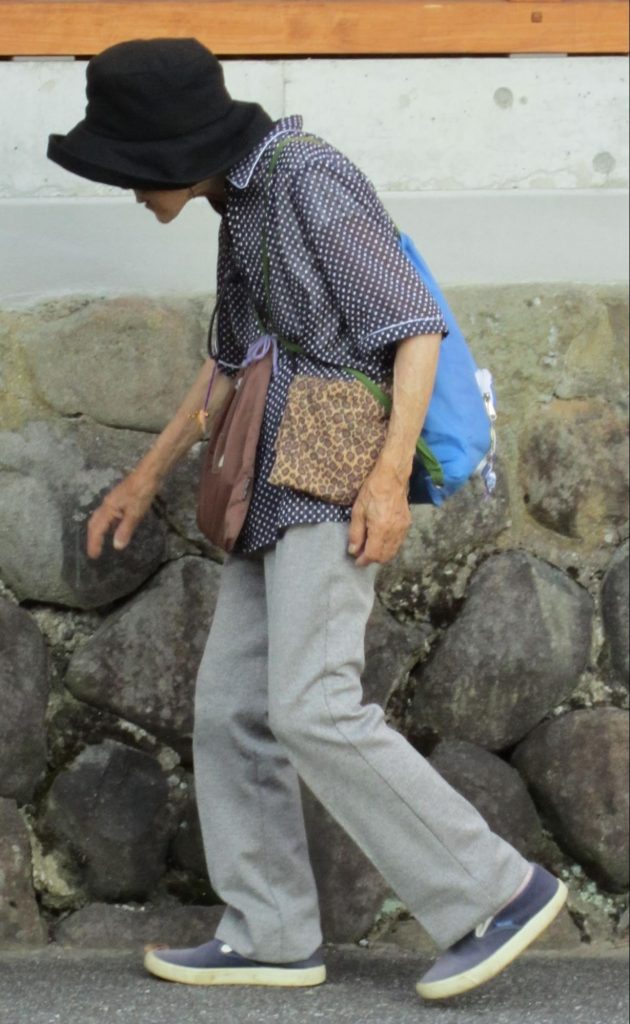
Image by James Heilman, MD / CC BY-SA 3.0
Calcium inadequacy is most prevalent in adolescent girls and the elderly. Proper dietary intake of calcium is critical for proper bone health.
Despite the wealth of evidence supporting the many health benefits of calcium (particularly bone health), the average American diet falls short of achieving the recommended dietary intakes of calcium. In fact, in females older than nine years of age, the average daily intake of calcium is only about 70 percent of the recommended intake. Here we will take a closer look at particular groups of people who may require extra calcium intake.
- Adolescent teens. A calcium-deficient diet is common in teenage girls as their dairy consumption often considerably drops during adolescence.
- Amenorrheic women and the ““. Amenorrhea refers to the absence of a menstrual cycle. Women who fail to menstruate suffer from reduced estrogen levels, which can disrupt and have a negative impact on the calcium balance in their bodies. The “female athlete triad” is a combination of three conditions characterized by amenorrhea, disrupted eating patterns, and . Exercise-induced amenorrhea and anorexia nervosa-related amenorrhea can decrease bone mass.[2][3] In female athletes, as well as active women in the military, low BMD, menstrual irregularities, and individual dietary habits together with a history of previous stress issues are related to an increased susceptibility to future stress fractures.[4][5]
- The elderly. As people age, calcium is reduced, the kidneys lose their capacity to convert vitamin D to its most active form, the kidneys are no longer efficient in retaining calcium, the skin is less effective at synthesizing vitamin D, there are changes in overall dietary patterns, and older people tend to get less exposure to sunlight. Thus the risk for calcium inadequacy is great.[6]
- Postmenopausal women. Estrogen enhances calcium absorption. The decline in this hormone during and after puts postmenopausal women especially at risk for calcium deficiency. Decreases in estrogen production are responsible for an increase in bone resorption and a decrease in calcium absorption. During the first years of menopause, annual decreases in bone mass range from 3–5 percent. After age sixty-five, decreases are typically less than 1 percent.[7]
- Lactose-intolerant people. Groups of people, such as those who are lactose intolerant, or who adhere to diets that avoid dairy products, may not have an adequate calcium intake.
- Vegans. Vegans typically absorb reduced amounts of calcium because their diets favor plant-based foods that contain oxalates and phytates.[8]
In addition, because vegans avoid dairy products, their overall consumption of calcium-rich foods may be less.
If you are lactose intolerant, have a milk allergy, are a vegan, or you simply do not like dairy products, remember that there are many plant-based foods that have a good amount of calcium and there are also some low-lactose and lactose-free dairy products on the market.
Calcium Supplements: Which One to Buy?
Many people choose to fulfill their daily calcium requirements by taking calcium supplements. Calcium supplements are sold primarily as calcium carbonate, calcium citrate, calcium lactate, and calcium phosphate, with elemental calcium contents of about 200 milligrams per pill. It is important to note that calcium carbonate requires an acidic environment in the stomach to be used effectively. Although this is not a problem for most people, it may be for those on medication to reduce stomach-acid production or for the elderly who may have a reduced ability to secrete acid in the stomach. For these people, calcium citrate may be a better choice. Otherwise, calcium carbonate is the cheapest. The body is capable of absorbing approximately 30 percent of the calcium from these forms.
Beware of Lead
There is public health concern about the lead content of some brands of calcium supplements, as supplements derived from natural sources such as oyster shell, bone meal, and dolomite (a type of rock containing calcium magnesium carbonate) are known to contain high amounts of lead. In one study conducted on twenty-two brands of calcium supplements, it was proven that eight of the brands exceeded the acceptable limit for lead content. This was found to be the case in supplements derived from oyster shell and refined calcium carbonate. The same study also found that brands claiming to be lead-free did, in fact, show very low lead levels. Because lead levels in supplements are not disclosed on labels, it is important to know that products not derived from oyster shell or other natural substances are generally low in lead content. In addition, it was also found that one brand did not disintegrate as is necessary for absorption, and one brand contained only 77 percent of the stated calcium content.[9]
Diet, Supplements, and Chelated Supplements
In general, calcium supplements perform to a lesser degree than dietary sources of calcium in providing many of the health benefits linked to higher calcium intake. This is partly attributed to the fact that dietary sources of calcium supply additional nutrients with health-promoting activities. It is reported that chelated forms of calcium supplements are easier to absorb as the chelation process protects the calcium from oxalates and phytates that may bind with the calcium in the intestines. However, these are more expensive supplements and only increase calcium absorption up to 10 percent. In people with low dietary intakes of calcium, calcium supplements have a negligible benefit on bone health in the absence of a vitamin D supplement. However, when calcium supplements are taken along with vitamin D, there are many benefits to bone health: is increased in early adulthood, BMD is maintained throughout adulthood, the risk of developing osteoporosis is reduced, and the incidence of fractures is decreased in those who already had osteoporosis. Calcium and vitamin D pills do not have to be taken at the same time for effectiveness. But remember that vitamin D has to be activated and in the bloodstream to promote calcium absorption. Thus, it is important to maintain an adequate intake of vitamin D.
The Calcium Debate
A recent study published in the British Medical Journal reported that people who take calcium supplements at doses equal to or greater than 500 milligrams per day in the absence of a vitamin D supplement had a 30 percent greater risk for having a heart attack.[10]
Does this mean that calcium supplements are bad for you? If you look more closely at the study, you will find that 5.8 percent of people (143 people) who took calcium supplements had a heart attack, but so did 5.5 percent of the people (111) people who took the placebo. While this is one study, several other large studies have not shown that calcium supplementation increases the risk for cardiovascular disease. While the debate over this continues in the realm of science, we should focus on the things we do know:
- There is overwhelming evidence that diets sufficient in calcium prevent osteoporosis and cardiovascular disease.
- People with risk factors for osteoporosis are advised to take calcium supplements if they are unable to get enough calcium in their diet. The National Osteoporosis Foundation advises that adults age fifty and above consume 1,200 milligrams of calcium per day. This includes calcium both from dietary sources and supplements.
- Consuming more calcium than is recommended is not better for your health and can prove to be detrimental. Consuming too much calcium at any one time, be it from diet or supplements, impairs not only the absorption of calcium itself, but also the absorption of other essential , such as iron and zinc. Since the GI tract can only handle about 500 milligrams of calcium at one time, it is recommended to have split doses of calcium supplements rather than taking a few all at once to get the of calcium.
Dietary Reference Intake for Calcium
The recommended dietary allowances (RDA) for calcium are listed in Table 10.1 “Dietary Reference Intakes for Calcium”. The RDA is elevated to 1,300 milligrams per day during adolescence because this is the life stage with accelerated bone growth. Studies have shown that a higher intake of calcium during increases the total amount of bone tissue that accumulates in a person. For women above age fifty and men older than seventy-one, the RDAs are also a bit higher for several reasons including that as we age, calcium absorption in the gut decreases, vitamin D3 activation is reduced, and maintaining adequate blood levels of calcium is important to prevent an acceleration of bone tissue loss (especially during menopause). Currently, the dietary intake of calcium for females above age nine is, on average, below the RDA for calcium. The Institute of Medicine (IOM) recommends that people do not consume over 2,500 milligrams per day of calcium as it may cause adverse effects in some people.
Children (1–3 years)7002,500
| Age Group | RDA (mg/day) | UL (mg/day) |
|---|---|---|
| Infants (0–6 months) | 200* | – |
| Infants (6–12 months) | 260* | – |
| Children (4–8 years) | 1,000 | 2,500 |
| Children (9–13 years) | 1,300 | 2,500 |
| Adolescents (14–18 years) | 1,300 | 2,500 |
| Adults (19–50 years) | 1,000 | 2,500 |
| Adult females (50–71 years) | 1,200 | 2,500 |
| Adults, male & female (> 71 years) | 1,200 | 2,500 |
| * denotes Adequate Intake |
Source: Ross AC, Manson JE, et al. The 2011 Report on Dietary Reference Intakes for Calcium and Vitamin D from the Institute of Medicine: What Clinicians Need to Know. J Clin Endocrinol Metab. 2011; 96(1), 53–8. http://www.ncbi.nlm.nih.gov/pubmed/21118827. Accessed October 10, 2017.
Dietary Sources of Calcium
In the typical American diet, calcium is obtained mostly from dairy products, primarily cheese. A slice of cheddar or Swiss cheese contains just over 200 milligrams of calcium. One cup of nonfat milk contains approximately 300 milligrams of calcium, which is about a third of the RDA for calcium for most adults. Foods fortified with calcium such as cereals, soy milk, and orange juice also provide one third or greater of the calcium RDA. Although the typical American diet relies mostly on dairy products for obtaining calcium, there are other good non-dairy sources of calcium.
Tools for Change
If you need to increase calcium intake, are a vegan, or have a to dairy products, it is helpful to know that there are some plant-based foods that are high in calcium. Tofu (made with calcium sulfate), turnip greens, mustard greens, and chinese cabbage are good sources. For a list of non-dairy sources you can find the calcium content for thousands of foods by visiting the USDA National Nutrient Database (http://www.nal.usda.gov/fnic/foodcomp/search/). When obtaining your calcium from a vegan diet, it is important to know that some plant-based foods significantly impair the absorption of calcium. These include spinach, Swiss chard, rhubarb, beets, cashews, and peanuts. With careful planning and good selections, you can ensure that you are getting enough calcium in your diet even if you do not drink milk or consume other dairy products.
Calcium Bioavailability
In the small intestine, calcium absorption primarily takes place in the duodenum (first section of the small intestine) when intakes are low, but calcium is also absorbed passively in the jejunum and ileum (second and third sections of the small intestine), especially when intakes are higher. The body doesn’t completely absorb all the calcium in food. Interestingly, the calcium in some vegetables such as kale, brussel sprouts, and bok choy is better absorbed by the body than are dairy products. About 30 percent of calcium is absorbed from milk and other dairy products.
The greatest positive influence on calcium absorption comes from having an adequate intake of vitamin D. People deficient in vitamin D absorb less than 15 percent of calcium from the foods they eat. The hormone estrogen is another factor that enhances calcium bioavailability. Thus, as a woman ages and goes through menopause, during which estrogen levels fall, the amount of calcium absorbed decreases and the risk for bone disease increases. Some fibers, such as inulin, found in jicama, onions, and garlic, also promote calcium intestinal uptake.
Chemicals that bind to calcium decrease its bioavailability. These negative effectors of calcium absorption include the oxalates in certain plants, the tannins in tea, phytates in nuts, seeds, and grains, and some fibers. Oxalates are found in high concentrations in spinach, parsley, cocoa, and beets. In general, the calcium bioavailability is inversely correlated to the oxalate content in foods. High-fiber, low-fat diets also decrease the amount of calcium absorbed, an effect likely related to how fiber and fat influence the amount of time food stays in the gut. Anything that causes diarrhea, including sickness, medications, and certain symptoms related to old age, decreases the transit time of calcium in the gut and therefore decreases calcium absorption. As we get older, stomach acidity sometimes decreases, diarrhea occurs more often, kidney function is impaired, and vitamin D absorption and activation is compromised, all of which contribute to a decrease in calcium bioavailability.
| Food | Serving | Calcium (mg) | Absorption (%) | Estimated Calcium Absorbed (mg) | % Daily Value1 | % Daily Value2 |
|---|---|---|---|---|---|---|
| Yogurt, low fat | 8.5 oz. | 300 | 32 | 96 | 7.4 | 9.6 |
| Mozzarella, part skim | 1.5 oz. | 333 | 32 | 107 | 8.2 | 10.7 |
| Sardines, canned with bones | 3 oz. | 325 | 27 | 88 | 6.8 | 8.8 |
| Cheddar Cheese | 1.5 oz. | 303 | 32 | 97 | 7.5 | 9.7 |
| Milk, nonfat | 8.5 oz. | 300 | 32 | 96 | 7.4 | 9.6 |
| Soymilk, calcium fortified | 8.5 oz. | 300 | 24 | 72 | 5.5 | 7.2 |
| Orange juice, calcium fortified | 8.5 oz. | 300 | 36 | 109 | 8.4 | 10.9 |
| Tofu, firm, made with calcium sulfate | ½ c. | 258 | 31 | 80 | 6.2 | 8.0 |
| Salmon, canned with bones | 3 oz. | 181 | 27 | 49 | 3.8 | 4.9 |
| Turnip Greens | ½ c. | 99 | 52 | 51 | 4.0 | 5.1 |
| Kale, cooked | 1 c. | 94 | 49 | 30 | 2.3 | 3.0 |
| Vanilla Ice Cream, light | ½ c. | 84 | 32 | 27 | 2.1 | 2.7 |
| Broccoli, cooked | 1 c. | 35 | 61 | 19 | 1.5 | 1.9 |
| Cauliflower, cooked | 1 c. | 10 | 69 | 6.9 | 0.5 | 0.7 |
| Red Beans, cooked | 1 c. | 41 | 24 | 9.84 | 0.8 | 1.0 |
1Based on DV = 1000 mg
2Based on DV = 1300 mg
Source:
Office of Dietary Supplements. (2020, March 26). Calcium. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
Titchenal, C. A., & Dobbs, J. (2007). A system to assess the quality of food sources of calcium. Journal of Food Composition and Analysis, 20(8), 717–724. doi: 10.1016/j.jfca.2006.04.013
Learning Activities
Technology Note: The second edition of the Human Nutrition Open Educational Resource (OER) textbook features interactive learning activities. These activities are available in the web-based textbook and not available in the downloadable versions (EPUB, Digital PDF, Print_PDF, or Open Document).
Learning activities may be used across various mobile devices, however, for the best user experience it is strongly recommended that users complete these activities using a desktop or laptop computer.
- Birkett NJ. (1998). Comments on a Meta-Analysis of the Relation between Dietary Calcium Intake and Blood Pressure. American Journal of Epidemiology, 148(3), 223–28. http://aje.oxfordjournals.org/content/148/3/223.long. Accessed October 10, 2017. ↵
- Drinkwater B, Bruemner B, Chesnut C. (1990). Menstrual History As a Determinant of Current Bone Density in Young Athletes. The Journal of the American Medical Association, 263(4), 545–8. http://www.ncbi.nlm.nih.gov/pubmed/2294327?dopt=Abstract. . Accessed November 22, 2017. ↵
- Marcus R. et al. (1985). Menstrual Function and Bone Mass in Elite Women Distance Runners: Endocrine and Metabolic Features. The Annuals of Internal Medicine, 102(2), 58–63. http://www.ncbi.nlm.nih.gov/pubmed/3966752?dopt=Abstract. Accessed November 22, 2017. ↵
- Nattiv A. Stress (2000). Fractures and Bone Health in Track and Field Athletes. The Journal of Science & Medicine in Sport, 3(3), 268–79. http://www.ncbi.nlm.nih.gov/pubmed/11101266?dopt=Abstract.,.Accessed November 22, 2017. ↵
- Johnson AO, et al. (1993). Correlation of Lactose Maldigestion, Lactose Intolerance, and Milk Intolerance. American Journal of Clinical Nutrition, 57(3), 399–401. http://www.ncbi.nlm.nih.gov/pubmed/8438774?dopt=Abstract. Accessed November 22, 2017. ↵
- Calcium and Vitamin D in the Elderly. International Osteoporosis Foundation. http://www.iofbonehealth.org/patients-public/about-osteoporosis/prevention /nutrition/calcium-and-vitamin-d-in-the-elderly.html. Published 2012. Accessed November 22, 2017. ↵
- Daniels CE. (2000). Estrogen Therapy for Osteoporosis Prevention in Postmenopausal Women. National Institute of Health: Pharmacy. Update March/April 2000. ↵
- Dietary Reference Intakes for Calcium and Vitamin D.Food and Nutrition Board, Institute of Medicine. Washington, DC: National Academy Press. 2010. ↵
- Ross EA, Szabo NJ, Tebbett IR. (2000). Lead Content of Calcium Supplements. The Journal of the American Medical Association, 284, 1425–33. ↵
- Bolland MJ. et al. (2010). Effect of Calcium Supplements on Risk of Myocardial Infarction and Cardiovascular Events: Meta-Analysis. British Medical Journal, 341(c3691). ↵
The major structural and supportive connective tissue of the body.
The process where bone is broken down and releases calcium into the blood.
A hormone secreted by the pancreas in response to elevated blood glucose levels to transport glucose into the muscle or fat cells.
A hormone that acts to increase blood calcium levels and is released from the parathyroid gland.
(Parathyroid Hormone) A hormone that acts to increase blood calcium levels and is released from the parathyroid gland.
A hormone that stimulates bone mineralization and inhibits bone breakdown which is produced in the thyroid gland.
A protein molecule that speeds up or accelerates specific chemical reactions without changing itself.
A fat-soluble vitamin that can be made in the body when there is exposure to sunlight and is needed for the absorption of calcium.
A gland located in the neck that produces both thyroid hormone and calcitonin.
The combination of energy restrictive diet, changes in hormone levels which affect menstruation, and low bone mineral density that may occur in female athletes.
A disorder affecting the bones that is characterized as a loss in bone mass, increased bone fragility, and increased risk of fractures.
The amount of a dietary nutrient that is absorbed and utilized by the body.
The time in a woman’s life where the menstrual cycle ends.
The maximum bone density attained at any time in life that usually occurs in adulthood.
An element used in the body to promote chemical reactions and help form body structures.
(Recommended Dietary Allowance) The levels of intake of essential nutrients that is based off of scientific knowledge, and it judged by the Food and Nutrition Board to be adequate to meet the known nutrient needs for all healthy people.
A period of sexual maturity where rapid growth and physical changes occur.
An adverse immune response to specific protein.
