Weight Management

“” is a word that has sprung up in the language of public health professionals in the last two decades. The Centers for Disease Control and Prevention (CDC) defines obesogenic as “an environment that promotes increased food intake, non-healthful foods, and physical inactivity.”[1]
The CDC reports that in 2009 in the United States, 33 percent of adults and 16 percent of children were obese, a doubling and tripling of the numbers since 1980, respectively, while in Hawai‘i the obesity rate was 23.8% in 2016 with 40.8% of those individuals being Native Hawaiians.[2]
The health consequences of too much body fat are numerous, including increased risks for cardiovascular disease, Type 2 diabetes, and some cancers. The medical costs related to obesity are well over one hundred billion dollars and in Hawai‘i, over $470 million is spent annually. On the individual level, people who are obese spend $1,429 more per year for medical care than people of healthy .
Numerous obesogenic agents that contribute to this immense public health problem have become a part of everyday life in American society. The fast food industry has been growing for decades and continues to grow despite the latest economic slump. In America today there are over twelve thousand McDonald’s restaurants, while in 1960 there was one. Food portions have been getting bigger since the 1960s, and in the 1990s North American society experienced the “super-size” marketing boom, which still endures. Between 1960 and 2000 more than 123 million vehicles were added to the American society. Escalators, elevators, and horizontal walkways now dominate shopping malls and office buildings, factory work has become increasingly mechanized and robotized, the typical American watches more than four hours of television daily, and in many work places the only tools required to conduct work are a chair and a computer. The list of all the societal obesogenic factors goes on and on. They are the result of modernization, industrialization, and urbanization continuing on without individuals, public health officials, or government adequately addressing the concurrent rise in overweight and obesity.
With obesity at epidemic proportions in America it is paramount that policies be implemented or reinforced at all levels of society, and include education, agriculture, industry, urban planning, healthcare, and government. Reversing and stopping obesity are two different things. The former will require much more societal and individual change than the latter. The following are some ideas for constructing an environment in America that promotes health and confronts the obesity epidemic:
Individual Level
- Purchase less prepared foods and eat more whole foods.
- Decrease portion sizes when eating or serving food.
- Eat out less, and when you do eat out choose low- options.
- Walk or bike to work. If this is not feasible, walk while you are at work.
- Take the stairs when you come upon them or better yet, seek them out.
- Walk your neighborhood and know your surroundings. This benefits both health and safety.
- Watch less television.
Community Level
- Request that your college/workplace provides more access to healthy low-cost foods.
- Support changes in school lunch programs.
- Participate in cleaning up local green spaces and then enjoy them during your leisure time.
- Patronize local farms and fruit-and-vegetable stands.
- Talk to your grocer and ask for better whole-food choices and seafood at a decent price.
- Ask the restaurants you frequently go to, to serve more nutritious food and to accurately display calories of menu items.
National Level
- Support policies that increase the walkability of cities.
- Support national campaigns addressing obesity, such as America on the Move.
- Support policies that support local farmers and the increased access and affordability of healthy food.
Some scientists predict that the childhood obesity rate will reach 100 percent by 2044. It is critical for the nation’s health to change our environment to one that promotes weight loss and/or weight maintenance. However, action is needed on multiple fronts to reverse the obesity epidemic trend within one generation.
In this section you will learn how to assess body weight and fatness. You will also learn that it is not only society and environment that play a role in body weight and fatness, but also physiology, genetics, and behavior—and that all of them interact. We will also discuss the health risks of being underweight and overweight, learn evidence-based solutions to maintain body weight at the individual level, and assess the current state of affairs of combating the obesity epidemic in the United States.
Balancing Energy Input with Energy Output

To Maintain Weight, Energy Intake Must Balance Energy Output
Recall that the macronutrients you consume are either converted to , stored, or used to synthesize macromolecules. A nutrient’s metabolic path is dependent upon . When you are in a positive energy balance the excess nutrient energy will be stored or used to grow (e.g., during childhood, pregnancy, and wound healing). When you are in negative energy balance you aren’t taking in enough energy to meet your needs, so your body will need to use its stores to provide energy. Energy balance is achieved when intake of energy is equal to energy expended. Weight can be thought of as a whole body estimate of energy balance; body weight is maintained when the body is in energy balance, lost when it is in negative energy balance, and gained when it is in positive energy balance. In general, weight is a good predictor of energy balance, but many other factors play a role in energy intake and energy expenditure. Some of these factors are under your control and others are not. Let us begin with the basics on how to estimate energy intake, energy requirement, and energy output. Then we will consider the other factors that play a role in maintaining energy balance and hence, body weight.
Estimating Energy Requirement
To maintain body weight you have to balance the calories obtained from food and beverages with the calories expended every day. Here, we will discuss how to calculate your energy needs in kilocalories per day so that you can determine whether your caloric intake falls short, meets, or exceeds your energy needs. The Institute of Medicine has devised a formula for calculating your (). It takes into account your age, sex, weight, height, and physical activity level (PA). The EER is a standardized mathematical prediction of a person’s daily energy needs in kilocalories per day required to maintain weight. It is calculated for those over 18 years of age via the following formulas:
Adult male: EER = 662 − [9.53 X age (y)] + PA X [15.91 X wt (kg) + 5.39.6 X ht (m)]
Adult female: EER = 354 − [6.91 x age (y)] + PA x [9.36 x wt (kg) + 726 x ht (m)]
Note: to convert pounds to kilograms, divide weight in pounds by 2.2. To convert feet to meters, divide height in feet by 3.3.
Estimating Caloric Intake
To begin your dietary assessment, go to MyPlate, which is available on the (USDA) website: http://www.choosemyplate.gov/.
| Activity Level | Men PA Value | Women PA Value | Description |
|---|---|---|---|
| Sedentary | 1.00 | 1.00 | No physical activity beyond that required for independent living |
| Low | 1.11 | 1.12 | Equivalent to walking 1.5 to 3 miles per day |
| Moderate | 1.25 | 1.27 | Equivalent to walking 3 to 10 miles per day |
| High | 1.48 | 1.45 | Equivalent to walking 10 or more miles per day |
| These values only apply to normal weight adults and not to children or pregnant or lactating women. |
These values only apply to normal weight adults and not to children or pregnant or lactating women.
The numbers within the equations for the EER were derived from measurements taken from a group of people of the same sex and age with similar body size and physical activity level. These standardized formulas are then applied to individuals whose measurements have not been taken, but who have similar characteristics, in order to estimate their energy requirements. Thus, a person’s EER is, as the name suggests, an estimate for an average person of similar characteristics. EER values are different for children, pregnant or lactating women, and for overweight and obese people. Also, remember the EER is calculated based on weight maintenance, not for weight loss or weight gain.
The 2015 Dietary Guidelines provides a table (Table 8.3 “Estimated Daily Calorie Needs”) that gives the estimated daily calorie needs for different age groups of males and females with various activity levels. The Dietary Guidelines also states that while knowing the number of calories you need each day is useful, it is also pertinent to obtain your calories from foods and consume the various macronutrients in their (AMDRs) (Table 8.4 “Acceptable Macronutrient Distribution Ranges”).
| Sex | Age (years) | Sedentary | Moderately Active | Active |
|---|---|---|---|---|
| Child (female and male) | 2–3 | 1,000 | 1,000–1,400 (male)1,000-1,200 (female) | 1,000–1,400 |
| Female | 4–8 | 1,200–1,400 | 1,400–1,600 | 1,400–1,800 |
| Female | 9–13 | 1,400–1,600 | 1,600–2,000 | 1,800–2,200 |
| Female | 14–18 | 1,800 | 2,000 | 2,400 |
| Female | 19–30 | 1,800–2,000 | 2,000–2,200 | 2,400 |
| Female | 31–50 | 1,800 | 2,000 | 2,200 |
| Female | 51+ | 1,600 | 1,800 | 2,000–2,200 |
| Male | 4–8 | 1,200–1,400 | 1,400–1,600 | 1,600–2,000 |
| Male | 9–13 | 1,600–2,000 | 1,800–2,200 | 2,000–2,600 |
| Male | 14–18 | 2,000–2,400 | 2,400–2,800 | 2,800–3,200 |
| Male | 19–30 | 2,400–2,600 | 2,600–2,800 | 3,000 |
| Male | 31–50 | 2,200–2,400 | 2,400–2,600 | 2,800–3,000 |
| Male | 51+ | 2,000–2,200 | 2,200–2,400 | 2,400–2,800 |
Source: 2010 Dietary Guidelines for Americans. US Department of Agriculture. http://health.gov/dietaryguidelines/dga2010/DietaryGuidelines2010.pdf. Published 2010. Accessed September 22, 2017.
| Age | Carbohydrates (% of Calories) | Protein (% of Calories) | Fat (% of Calories) |
|---|---|---|---|
| Young Children (1–3) | 45–65 | 5–20 | 30–40 |
| Older children/adolescents (4–18) | 45–65 | 10–30 | 25–35 |
| Adults (19 and older) | 45–65 | 10–35 | 20–35 |
Source: Dietary Reference Intakes: Macronutrients.” Dietary Reference Intakes for Energy, Carbohydrate. Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Institute of Medicine. http://nationalacademies.org/hmd/~/media/Files/Activity%20Files/Nutrition/DRI-Tables/8_Macronutrient%20Summary.pdf?la=en. Accessed September 22, 2017.
Total Energy Expenditure (Output)
The amount of energy you expend every day includes not only the calories you burn during physical activity, but also the calories you burn while at rest (basal ), and the calories you burn when you digest food. The sum of caloric expenditure is referred to as (). Basal metabolism refers to those metabolic pathways necessary to support and maintain the body’s basic functions (e.g. breathing, heartbeat, liver and kidney function) while at rest. The () is the amount of energy required by the body to conduct its basic functions over a certain time period. The great majority of energy expended (between 50 and 70 percent) daily is from conducting life’s basic processes. Of all the organs, the liver requires the most energy (Table 8.5 “Energy Breakdown of Organs”). Unfortunately, you cannot tell your liver to ramp up its activity level to expend more energy so you can lose weight. BMR is dependent on body size, body composition, sex, age, nutritional status, and genetics. People with a larger frame size have a higher BMR simply because they have more mass. Muscle tissue burns more calories than fat tissue even while at rest and thus the more muscle mass a person has, the higher their BMR. Since females typically have less muscle mass and a smaller frame size than men, their BMRs are generally lower than men’s. As we get older muscle mass declines and thus so does BMR. Nutritional status also affects basal metabolism. Caloric restriction, as occurs while dieting, for example, causes a decline in BMR. This is because the body attempts to maintain homeostasis and will adapt by slowing down its basic functions to offset the decrease in energy intake. Body temperature and levels are additional determinants of BMR.
| Organ | Percent of Energy Expended |
|---|---|
| Liver | 27 |
| Brain | 19 |
| Heart | 7 |
| Kidneys | 10 |
| Skeletal muscle (at rest) | 18 |
| Other organs | 19 |
FAO/WHO/UNU, 1985.
Energy and Protein Requirements. World Health Organization Technical Report Series 724. http://www.fao.org/doCReP/003/aa040e/AA040E00.htm. Updated 1991. Accessed September 17, 2017.
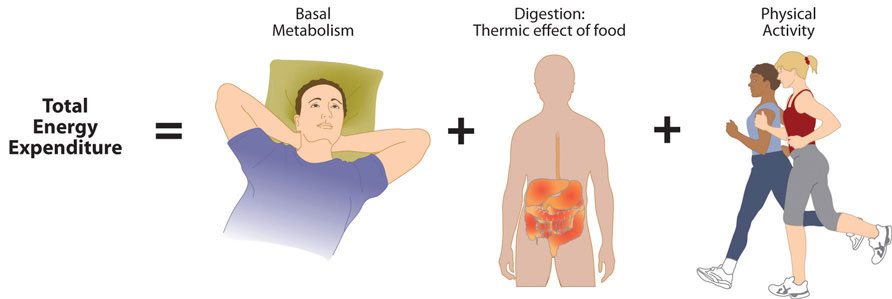
Total energy expenditure is the sum of energy expended at rest, during digestion, and during physical activity.
The energy required for all the enzymatic reactions that take place during food digestion and absorption of nutrients is called the “thermic effect of food” and accounts for about 10 percent of total energy expended per day. The other energy required during the day is for physical activity. Depending on lifestyle, the energy required for this ranges between 15 and 30 percent of total energy expended. The main control a person has over TEE is to increase physical activity.
How to Calculate Total Energy Expenditure
Calculating TEE can be tedious, but has been made easier as there are now calculators available on the Web. TEE is dependent on age, sex, height, weight, and physical activity level. The equations are based on standardized formulas produced from actual measurements on groups of people with similar characteristics. To get accurate results from web-based TEE calculators, it is necessary to record your daily activities and the time spent performing them. A spreadsheet for doing so is available online at http://www.health-calc.com/Calculate_daily_energy_expenditure.pdf. Health-calc.com offers an interactive TEE calculator. http://www.health-calc.com/diet/energy-expenditure-advanced
Learning Activities
Technology Note: The second edition of the Human Nutrition Open Educational Resource (OER) textbook features interactive learning activities. These activities are available in the web-based textbook and not available in the downloadable versions (EPUB, Digital PDF, Print_PDF, or Open Document).
Learning activities may be used across various mobile devices, however, for the best user experience it is strongly recommended that users complete these activities using a desktop or laptop computer.
- Obesogenic Environments. Center for Disease Control and Prevention (CDC). https://www.cdc.gov/pcd/issues/2015/14_0559.htm. Published 2013. Accessed September 22, 2017. ↵
- Hawaii State Obesity Data, Rates, and Trends. The State of Obesity: Better Policies for a Healthier America. https://stateofobesity.org/states/hi/. Published August 2017. Accessed September 22, 2017. ↵
- Dietary Reference Intake Tables.Health Canada. http://www.hc-sc.gc.ca/fn-an/nutrition/reference/table/index-eng.php#eeer. Updated November 29, 2010. Accessed September 22, 2017. ↵
An environment that promotes increased food intake, non-healthful foods, and physical inactivity
A body’s relative mass.
A fundamental unit of energy, equal to 4.1855 joule; 1000 calories equals 1 kcal.
The capacity of a body or physical system for doing work. There are two fundamental forms: kinetic energy and potential energy.
The state in which the total energy intake equals total energy needs.
The daily requirement for dietary energy intake that is predicted to maintain energy balance in healthy, normal weight individuals.
(Estimated Energy Requirement) The daily requirement for dietary energy intake that is predicted to maintain energy balance in healthy, normal weight individuals.
Government organization responsible for protecting the public health by ensuring the safety, efficacy, and security of human and veterinary drugs, biological products,and the nation's food supply, cosmetics, and products that emit radiation.
Food that is high in nutrients but relatively low in calories
A range of intakes for carbohydrates, fat, and protein expressed as a percentage of total energy intake for normal healthy individuals.
The entire biochemical activities of an organism.
The amount of energy that a person burns each day.
(Total Energy Expenditure) The amount of energy that a person burns each day.
The rate at which the body burns or uses energy while at rest to keep vital functions going.
(Basal Metabolic Rate) The rate at which the body burns or uses energy while at rest to keep vital functions going.
Hormones that are produced by the thyroid gland and regulate metabolic rate.
